March 2022 • DALLAS MEDICAL JOURNAL | 13
an incredible tool for functional evaluation
of normal anatomy as well as pathology.
Given the ability of the ultrasound to distinguish
alterations in relative echogenicity, by
depicting changes in density, composition,
and fl uid/fl ow state, ultrasonography can
not only detect disease but, in the hands of
a qualifi ed sonographer, it can consistently
and accurately assess disease severity. Additionally,
for the same reasons as above,
ultrasound has signifi cant use in monitoring
the healing process by visualizing the tissue
corrections and adaptations that occur during
recovery post-injury or post-procedure.
Regarding LE and ME, repetitive microtrauma
to the common extensor tendon
and common fl exor tendon origins, respectively,
results in localized rupture of individual
tendon fi bers. Due to the lack of blood fl ow
to these areas, the tendons do not have the
ability to regenerate tendinous collagen.
As such, the spontaneous “healing” of
these microtears occurs by replacing
tendon collagen fi bers with disorganized
scar tissue. This subsequently
alters the tendon composition, and the
diseased tendon appears darker (less
dense/less echogenic) on ultrasound.
In many cases, because of the disorganized
layering of scar tissue, along with
the exudative reparatory reaction that
is concomitantly involved, the tendon
will appear swollen or hypertrophied,
providing further proof of chronic
disease process. Further, as tendon
fi bers that anchor directly to bone are
repetitively stressed, the microtears
materializing at or near bony origin can lead
to cortical remodeling, seen as hyperechoic
(bright) cortical
irregularities.
Treatment
Although there are still no universally accepted
treatment modalities for these two
conditions, non-operative management
remains the mainstay of both. 90% of cases
of symptomatic LE signifi cantly resolve with
non-operative management, and there are
just slightly worse results for symptomatic
ME. The treatment of both conditions has 5
therapeutic goals: controlling elbow pain,
preserving movement of the aff ected arm,
improving grip strength and endurance, restoring
normal function of the aff ected arm,
and preventing further deterioration 1.
Non-operative treatment starts with
RICE (rest, ice, compression, and elevation)
during the initial painful stage followed by
activity modifi cation and physical therapy.
A well-put-together home exercise program
may be used once the acute stage has
improved, but having supervised physical
therapy sessions remains ideal. Modifi cations
to equipment such as lowering the tension
on strings and increasing grip size can help
those who play racket sports. A counterforce
brace can be used to disperse the stress on
the tension point of the common extensor/
fl exor tendon, and a neutral wrist splint can
help avoid too much wrist extension/fl exion
that may exacerbate symptoms. Additionally,
NSAIDs can be helpful with pain in both
topical (diclofenac gel) and oral (ibuprofen,
naproxen, etc.) forms.
If these measures do not signifi cantly
relieve or resolve symptoms within 3 to 6
months, more interventional non-operative
treatment modalities may be indicated.
There has been increasing evidence for extracorporeal
shockwave therapy (ESWT), especially
for LE. The exact mechanism of how
ESWT works is still unclear, but it is thought
that these sound waves provide transient
pressures that result in direct stimulation of
healing, neovascularization, direct suppressive
eff ects on nociceptors, and a hyperstimulation
mechanism blocking the gate control
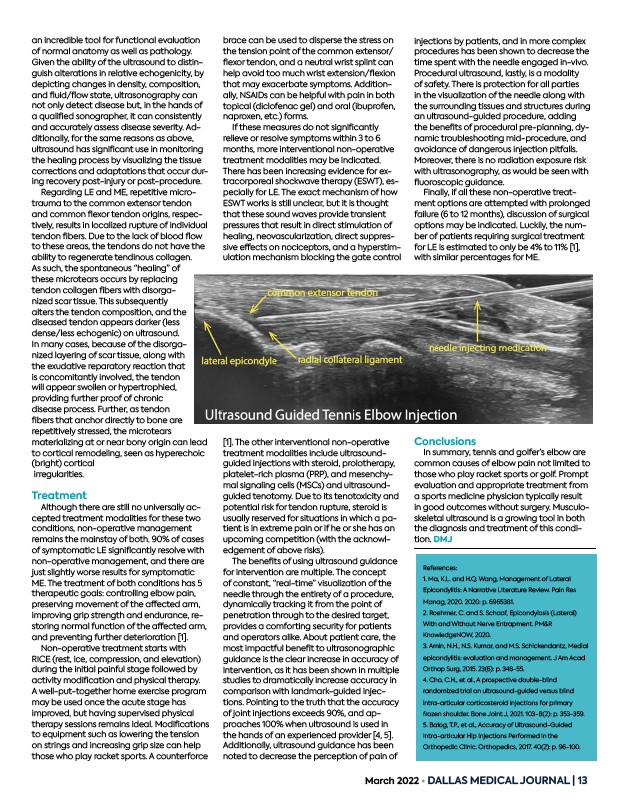
1. The other interventional non-operative
treatment modalities include ultrasoundguided
injections with steroid, prolotherapy,
platelet-rich plasma (PRP), and mesenchymal
signaling cells (MSCs) and ultrasoundguided
tenotomy. Due to its tenotoxicity and
potential risk for tendon rupture, steroid is
usually reserved for situations in which a patient
is in extreme pain or if he or she has an
upcoming competition (with the acknowledgement
of above risks).
The benefi ts of using ultrasound guidance
for intervention are multiple. The concept
of constant, “real-time” visualization of the
needle through the entirety of a procedure,
dynamically tracking it from the point of
penetration through to the desired target,
provides a comforting security for patients
and operators alike. About patient care, the
most impactful benefi t to ultrasonographic
guidance is the clear increase in accuracy of
intervention, as it has been shown in multiple
studies to dramatically increase accuracy in
comparison with landmark-guided injections.
Pointing to the truth that the accuracy
of joint injections exceeds 90%, and approaches
100% when ultrasound is used in
the hands of an experienced provider 4, 5.
Additionally, ultrasound guidance has been
noted to decrease the perception of pain of
injections by patients, and in more complex
procedures has been shown to decrease the
time spent with the needle engaged in-vivo.
Procedural ultrasound, lastly, is a modality
of safety. There is protection for all parties
in the visualization of the needle along with
the surrounding tissues and structures during
an ultrasound-guided procedure, adding
the benefi ts of procedural pre-planning, dynamic
troubleshooting mid-procedure, and
avoidance of dangerous injection pitfalls.
Moreover, there is no radiation exposure risk
with ultrasonography, as would be seen with
fl uoroscopic guidance.
Finally, if all these non-operative treatment
options are attempted with prolonged
failure (6 to 12 months), discussion of surgical
options may be indicated. Luckily, the number
of patients requiring surgical treatment
for LE is estimated to only be 4% to 11% 1,
with similar percentages for ME.
Conclusions
In summary, tennis and golfer’s elbow are
common causes of elbow pain not limited to
those who play racket sports or golf. Prompt
evaluation and appropriate treatment from
a sports medicine physician typically result
in good outcomes without surgery. Musculoskeletal
ultrasound is a growing tool in both
the diagnosis and treatment of this condition.
DMJ
References:
1. Ma, K.L. and H.Q. Wang, Management of Lateral
Epicondylitis: A Narrative Literature Review. Pain Res
Manag, 2020. 2020: p. 6965381.
2. Roehmer, C. and S. Schaaf, Epicondylosis (Lateral)
With and Without Nerve Entrapment. PM&R
KnowledgeNOW, 2020.
3. Amin, N.H., N.S. Kumar, and M.S. Schickendantz, Medial
epicondylitis: evaluation and management. J Am Acad
Orthop Surg, 2015. 23(6): p. 348-55.
4. Cho, C.H., et al., A prospective double-blind
randomized trial on ultrasound-guided versus blind
intra-articular corticosteroid injections for primary
frozen shoulder. Bone Joint J, 2021. 103-B(2): p. 353-359.
5. Balog, T.P., et al., Accuracy of Ultrasound-Guided
Intra-articular Hip Injections Performed in the
Orthopedic Clinic. Orthopedics, 2017. 40(2): p. 96-100.