NATIONAL BRAIN INJURY AWARENES S MONTH
TRAJECTORIES OF CHILDREN’S
EXECUTIVE FUNCTION AFTER
TRAUMATIC BRAIN INJURY
JAMA NETWORK. PEDIATRICS. MARCH 2021.
By Heather T. Keenan, MDCM, PhD, Amy E. Clark, MS,
Richard Holubkov, PhD, Charles S. Cox Jr, MD and Linda Ewing-Cobbs, PhD
Traumatic brain injury (TBI) can
adversely aff ect executive functions
(EFs) that play a central role
in both academic performance
and social interactions.1-4
Executive functions are self-regulation
skills that facilitate sustaining attention,
resisting distraction, managing frustration,
assessing the consequences of actions,
and planning for the future.5 Executive
functions develop by using neural networks
traversing frontal-striatal circuits,6 which
are frequently disrupted by TBI.7,8 Executive
function development extends
in a nonlinear fashion from
infancy into young adulthood,9
with EF components having different
developmental trajectories.
Inhibition and behavior
regulation accelerate rapidly
during preschool years and
continue to develop through
adolescence.5,10,11 Metacognitive
skills, such as working
memory, increase gradually,9
whereas planning accelerates
during late childhood and
adolescence.12 Because skills
in a rapid stage of development
may be more vulnerable
to disruption by TBI than more
well-established skills,13,14 TBI
sustained during periods of
accelerated EF growth may
be associated with greater
defi cit. Understanding how TBI
infl uences the developmental
trajectory of EF in children injured
in diff erent developmental
periods is critically important to
allow targeted intervention for
behavior regulation and metacognitive
skills.15
Executive functions are
commonly assessed using performancebased
measures and behavioral measures
of underlying EF. The Behavior Rating Inventory
of EF (BRIEF)16 is a parent-reported
behavioral measure widely used to provide
an ecological assessment of behavior regulation
and metacognitive EF in everyday
settings and may be particularly sensitive
to posttraumatic diffi culties.17 Prospective
studies using EF ratings over the fi rst 2
years after TBI consistently show a dosedependent
response: children with severe
TBI (sTBI) have greater executive dysfunction
than those with mild TBI (mTBI).18,19
Time course and extent of EF recovery are
not established, with reports at 10 years
postinjury showing mixed results.20,21 Some
studies suggest no recovery of 1 or more EF
components across the fi rst 2 years after
TBI,18,19,22 whereas others found gains.23
Persistent decrements in EF 5 to 7 years
postinjury in children with sTBI suggest
that even when recovery occurs, children’s
EFs do not return to their preinjury trajectory.
24,25
To our knowledge, most prior studies
have not followed children longitudinally
beyond 2 years after TBI, limiting our knowledge
of recovery patterns. The current
study fi lls this gap by modeling injury and
demographic factors infl uencing children’s
EF growth curves from baseline performance
through 3 years postinjury, while
accounting for preinjury abilities and family
environment.18,19,26 We hypothesized (1) a
dose-response relationship with TBI severity,
by which children with severe injury would
show greater initial decrement, improvement
across the fi rst year, and then deceleration;
24 | DALLAS MEDICAL JOURNAL • March 2022
(2) that sex and age at injury would
moderate the eff ect of TBI, with girls having
greater diffi culties over time and greater
disruption of abilities rapidly developing at
the time of injury; and (3) that positive family
function and social capital would provide
a protective recovery eff ect.
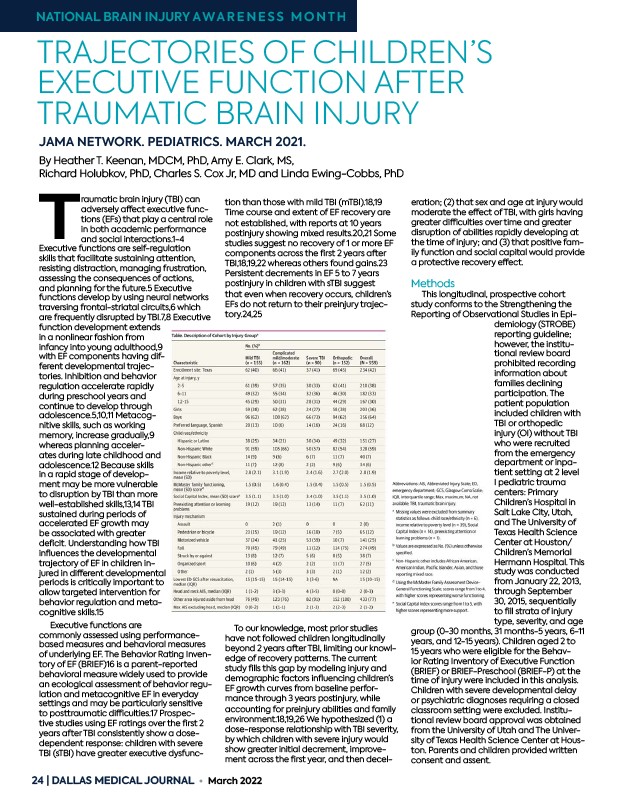
Methods
This longitudinal, prospective cohort
study conforms to the Strengthening the
Reporting of Observational Studies in Epidemiology
(STROBE)
reporting guideline;
however, the institutional
review board
prohibited recording
information about
families declining
participation. The
patient population
included children with
TBI or orthopedic
injury (OI) without TBI
who were recruited
from the emergency
department or inpatient
setting at 2 level
I pediatric trauma
centers: Primary
Children’s Hospital in
Salt Lake City, Utah,
and The University of
Texas Health Science
Center at Houston/
Children’s Memorial
Hermann Hospital. This
study was conducted
from January 22, 2013,
through September
30, 2015, sequentially
to fi ll strata of injury
type, severity, and age
group (0-30 months, 31 months-5 years, 6-11
years, and 12-15 years). Children aged 2 to
15 years who were eligible for the Behavior
Rating Inventory of Executive Function
(BRIEF) or BRIEF-Preschool (BRIEF-P) at the
time of injury were included in this analysis.
Children with severe developmental delay
or psychiatric diagnoses requiring a closed
classroom setting were excluded. Institutional
review board approval was obtained
from the University of Utah and The University
of Texas Health Science Center at Houston.
Parents and children provided written
consent and assent.