TBI, a challenge for the neurotrauma field
in examining multiple biomarkers including
markers from different modalities for effective
joint benefit.
Although this field is in its infancy, a few studies
have begun to explore combining biomarkers
for TBI. One study evaluated a panel
of blood-based biomarkers with and without
neuroimaging findings (CT and MRI) and
whether it discriminates between patients
with suspected mTBI using single-molecule
array technology.208 The panel included
GFAP, tau, UCH-L1, and NfL. Combining GFAP,
tau, and NfL showed satisfactory discriminatory
power in relating to MRI-detected
abnormalities, even in mTBI patients with a
normal CT. This study highlights the potential
of a multi-modal approach to guide future
clinical trials to improve medical decision
making, facilitate the use of MRI scanning,
and stratify patients with brain injuries.
Other studies that have examined
multiple biomarkers include those confirming
proteomic trauma-release proteomes
that identified a panel of astroglial injury
biomarkers.119 A panel that covers different
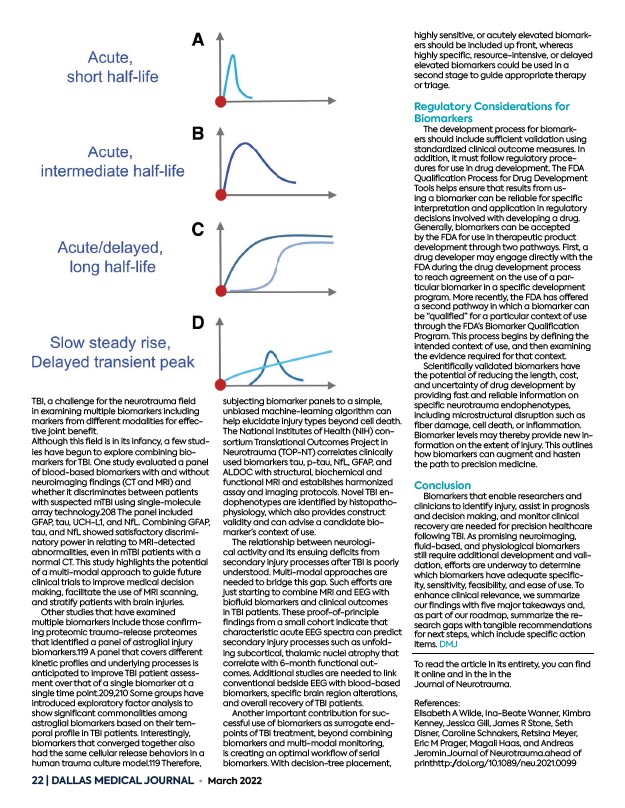
kinetic profiles and underlying processes is
anticipated to improve TBI patient assessment
over that of a single biomarker at a
single time point.209,210 Some groups have
introduced exploratory factor analysis to
show significant commonalities among
astroglial biomarkers based on their temporal
profile in TBI patients. Interestingly,
biomarkers that converged together also
had the same cellular release behaviors in a
human trauma culture model.119 Therefore,
subjecting biomarker panels to a simple,
unbiased machine-learning algorithm can
help elucidate injury types beyond cell death.
The National Institutes of Health (NIH) consortium
Translational Outcomes Project in
Neurotrauma (TOP-NT) correlates clinically
used biomarkers tau, p-tau, NfL, GFAP, and
ALDOC with structural, biochemical and
functional MRI and establishes harmonized
assay and imaging protocols. Novel TBI endophenotypes
22 | DALLAS MEDICAL JOURNAL • March 2022
are identified by histopathophysiology,
which also provides construct
validity and can advise a candidate biomarker’s
context of use.
The relationship between neurological
activity and its ensuing deficits from
secondary injury processes after TBI is poorly
understood. Multi-modal approaches are
needed to bridge this gap. Such efforts are
just starting to combine MRI and EEG with
biofluid biomarkers and clinical outcomes
in TBI patients. These proof-of-principle
findings from a small cohort indicate that
characteristic acute EEG spectra can predict
secondary injury processes such as unfolding
subcortical, thalamic nuclei atrophy that
correlate with 6-month functional outcomes.
Additional studies are needed to link
conventional bedside EEG with blood-based
biomarkers, specific brain region alterations,
and overall recovery of TBI patients.
Another important contribution for successful
use of biomarkers as surrogate endpoints
of TBI treatment, beyond combining
biomarkers and multi-modal monitoring,
is creating an optimal workflow of serial
biomarkers. With decision-tree placement,
highly sensitive, or acutely elevated biomarkers
should be included up front, whereas
highly specific, resource-intensive, or delayed
elevated biomarkers could be used in a
second stage to guide appropriate therapy
or triage.
Regulatory Considerations for
Biomarkers
The development process for biomarkers
should include sufficient validation using
standardized clinical outcome measures. In
addition, it must follow regulatory procedures
for use in drug development. The FDA
Qualification Process for Drug Development
Tools helps ensure that results from using
a biomarker can be reliable for specific
interpretation and application in regulatory
decisions involved with developing a drug.
Generally, biomarkers can be accepted
by the FDA for use in therapeutic product
development through two pathways. First, a
drug developer may engage directly with the
FDA during the drug development process
to reach agreement on the use of a particular
biomarker in a specific development
program. More recently, the FDA has offered
a second pathway in which a biomarker can
be “qualified” for a particular context of use
through the FDA’s Biomarker Qualification
Program. This process begins by defining the
intended context of use, and then examining
the evidence required for that context.
Scientifically validated biomarkers have
the potential of reducing the length, cost,
and uncertainty of drug development by
providing fast and reliable information on
specific neurotrauma endophenotypes,
including microstructural disruption such as
fiber damage, cell death, or inflammation.
Biomarker levels may thereby provide new information
on the extent of injury. This outlines
how biomarkers can augment and hasten
the path to precision medicine.
Conclusion
Biomarkers that enable researchers and
clinicians to identify injury, assist in prognosis
and decision making, and monitor clinical
recovery are needed for precision healthcare
following TBI. As promising neuroimaging,
fluid-based, and physiological biomarkers
still require additional development and validation,
efforts are underway to determine
which biomarkers have adequate specificity,
sensitivity, feasibility, and ease of use. To
enhance clinical relevance, we summarize
our findings with five major takeaways and,
as part of our roadmap, summarize the research
gaps with tangible recommendations
for next steps, which include specific action
items. DMJ
To read the article in its entirety, you can find
it online and in the in the
Journal of Neurotrauma.
References:
Elisabeth A Wilde, Ina-Beate Wanner, Kimbra
Kenney, Jessica Gill, James R Stone, Seth
Disner, Caroline Schnakers, Retsina Meyer,
Eric M Prager, Magali Haas, and Andreas
Jeromin.Journal of Neurotrauma.ahead of
printhttp:/doi.org/10.1089/neu.2021.0099